This post covers all aspects of histamine intolerance including its causes, symptoms, list of foods high in histamine, supplements and details of natural treatments to deal with excess of histamine I effectively use in clinic.
Did you know that we can’t really have a histamine free diet like we can have a gluten free diet? Find out why below.
Sleep plays a role in managing histamine intolerance so, as a bonus, I included a FREE download of my Sleep Guide: Top 3 Nutrition tips for better sleep tonight! Key nutrition tips for insomnia plus my top 3 bedtime snacks for deeper and restful sleep.
Lets get started!
Table of contents
What is histamine intolerance?
Histamine intolerance is a fairy common but under recognised and not fully understood problem linked with food sensitivities as well as gut and metabolic imbalances.
When a person has problems metabolising and breaking down histamine, its levels build up and lead to worrying symptoms such as hives, rashes and itching, swelling, abdominal pain, insomnia, fatigue and nasal congestion, among others (see more symptoms below).
Thus the symptoms are caused by having too much histamine circulating throughout the body rather than being histamine ‘intolerant’. This is important to realise and address using natural therapies and dietary strategies.
This disorder could be difficult to diagnose as it’s often confused with a number of other conditions that have similar symptoms, especially associated with food intolerances or allergies. In my practice I see this condition periodically, especially in clients with gut disorders, skin problems, headaches or migraines.
Let’s look at histamine intolerance more closely.
About histamine
Histamine is an amine (an organic nitrogen compound) produced by the immune system cells (mast cells, basophils and eosinophils) involved in the inflammatory immune response to an injury or foreign compounds. There is an emerging evidence that histamine producing bacteria in the gut is also a significant source of histamine. More on this below.
The normal inflammatory response is a healing mechanism that increases the permeability of capillaries (small blood vessels) to white blood cells so they can combat the pathogens or toxins present.
Histamine is also a neurotransmitter in the central nervous system (i.e. it relays messages between cells), where it’s involved in many brain functions such as arousal, pituitary hormone secretion, suppression of eating and cognitive functions. So we very much need histamine for the body to function well on many levels.
Histamine is also released in the body as part of an allergic reaction, causing the typical ‘itching, sneezing, wheezing, swelling’ symptoms. Nasal congestion is due to vasodilation (widening of blood vessels) and increased capillary permeability.
Enzyme diamine oxidase (DAO) breaks down histamine and maintains a histamine balance in the body. However, some people have a low level of this enzyme, and when they eat too many histamine-rich foods, they may suffer ‘allergy-like’ symptoms such as hives, headaches, rashes, itching, diarrhoea, vomiting or abdominal pain.
Histidine is also produced by some of the species of bacteria found in the gut. If they proliferate too much due to the gut flora imbalances (also known as gut dysbiosis or SIBO – small intestine bacterial overgrowth) they produce too much histamine and the symptoms appear.
This is one of the reasons why histamine intolerance is on the rise as an effect of alterations to our microbiota (gut flora) over the past 20 years or so, due to the changes to our diet. This includes a significant increase in the consumption of processed and packaged foods that are stored for a long time, use of additives and preservatives as well as pesticides and chemicals.
Causes of histamine intolerance
Overall, there are two main reasons for the symptoms to manifest:
1. Overproduction of histamine caused by:
- Gut dysbiosis/ SIBO (small intestine bacterial overgrowth) – one of the causes of histamine intolerance I see in practice is the imbalanced gut microbiome. Certain types of bacteria in the gut produce histamine and other types of bacteria degrade it maintaining balance. However, if there is more than required of the histamine producing bacteria, histamine excess will occur. Dysbiosis (bacterial imbalances in the gut) reduces histamine degradation AND increases histamine levels.
- Gut dysbiosis can also damage the intestinal lining (villi) responsible for production of enzymes including DAO which degrades histamine.
- Histamine-producing bacteria include: Lactobacillus casei, Lactobacillus delbrueckii, Lactobacillus bulgaricus, Lactobacillus reuteri, and Lactococcus lactis, Enterococcus faecalis, and various types of E. coli.
- Histamine-degrading bacteria include bifidobacteria species, particularly Bifidobacterium infantis, Bifidiobacterium breve, Bifidobacterium infants, Bifidobacterium longum, and also Lactobacillus Plantarum, Lactobacillus rhamnosus, Lactobacillus salivarius, and Lactobacillus gasseri.
- Research on probiotics continues so our knowledge is expending but it’s incomplete for now.
- Over activation of mast cells, which are the cells that largely produce histamine. We don’t fully understand what causes this at present.
2. Inability to break histamine down properly caused by:
- Impaired methylation – histamine N-methyltransferase enzyme (involved in histamine breakdown in the liver) requires methylation to function properly for it to work efficiently. Therefore compromised methylation will cause a decrease in the breakdown of histamine.
- Not enough histamine-degrading bacteria – which is related to gut dysbiosis (as stated above).
- Genetics – genetic defects involving two enzymes: diamine oxidase (DAO) or histamine N-methyltransferase which bind and breakdown histamine preventing excess. Some people don’t make enough of these enzymes because of faulty genes.
3. Many drugs have negative effects on microbiome. Some medications can facilitate histamine release, others can reduce the effectiveness of the DAO enzyme. As a result, the level of histamine rises and may cause symptoms, even in a person who has shown no signs of histamine intolerance in the past. Examples include:
- Some anti-histamines can cause constipation that increases a of developing SIBO (Small Intestine Bacterial Overgrowth).

- Common pain killers such as aspirin, non-steroidal anti-inflammatory drugs (NSAIDs) (19), some diuretics, antibiotics and antidepressants are among the medications that can affect the functioning of DAO (2).
- Metformin (diabetes drug) blocks the DAO enzyme and thus can cause histamine intolerance.
- Many other drugs including synthetic estrogen supplementation, some muscle relaxants and local anesthetics.
- Important: you should not stop any medicines without consulting with your doctor. You may be able to take the medication AND manage histamine intolerance through diet and other natural means.
4. Some people with adrenal fatigue who have cortisol production imbalances such as high cortisol, low cortisol or faulty production of cortisol throughout the day, are more likely to produce excess histamine. This is due to increased inflammation which triggers the release of histamine as a defence mechanism. Therefore dealing with adrenal fatigue is an important treatment step as well.
Symptoms of histamine intolerance
- Hives (urticaria)
- Itching (pruritis) – especially of the skin, eyes, ears, and nose
- Tissue swelling (angioedema) especially of facial and oral tissues and sometimes the throat, the latter causing the feeling of “throat tightening”
- Low blood pressure and fainting
- Getting dizzy when standing up quickly
- Rapid heartbeat / heart racing (tachycardia)
- Symptoms resembling anxiety or panic attack
- Chest pain
- Nasal congestion, runny nose, seasonal allergies
- Conjunctivitis – irritated, watery, reddened eyes
- Headaches and migraines
- Fatigue, irritability, insomnia
- Flushing and rosacea
- Blacking out / loss of consciousness for a few seconds unexplained by other causes
- Digestive tract issues especially heartburn (reflux), indigestion, non-gluten gut sensitivity, constipation and diarrhoea
Importantly, if someone has multiple allergic responses that are not associated with any particular trigger food(s) or allergy test results are negative, it could be a problem with histamine intolerance.
Please note that not all of the above symptoms occur in any single individual and the severity of symptoms varies, although the pattern seems to be consistent for each person.
Foods high in histamine (an overview)
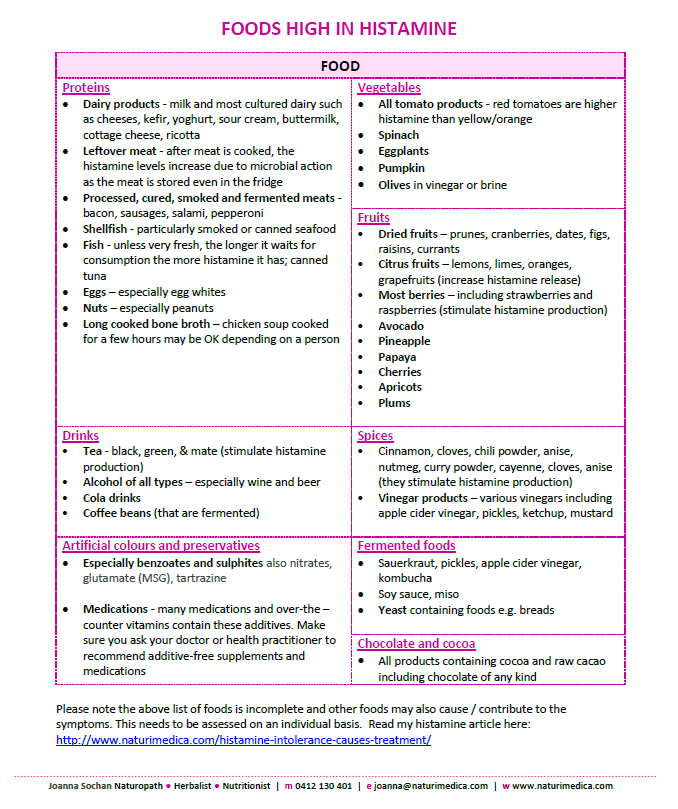
Please note the above list of foods is incomplete and other foods may also cause/ contribute to the symptoms. You can find a more comprehensive list of foods high and low in histamine.
Another excellent paper on histamine intolerance was published in August 2016 by Research Centers of Nutrition and Health (Grupo CINUSA) in Spain. The researchers conducted selective literature search for relevant publications in PubMed and other scientific data bases, combined with further data from the World Wide Web on histamine and other amines content in foods.
The paper includes comprehensive cross-checked tables of foods that are low, moderate and high in histamine. The researchers concluded that further studies are necessary to establish safety limits for bioactive amines in food, and the intolerance they may cause. A must read for all who have histamine intolerance symptoms.
Natural treatment options for histamine intolerance
- Testing – definitive testing for histamine intolerance has not been established as yet, although guidelines have been proposed. I don’t usually find testing is necessary in a clinical context as the gut and other symptoms, AND a person’s response to the low histamine diet are highly correlated with likely histamine intolerance.
- Healing the gut is the top priority – most people with histamine intolerance have damaged gut lining resulting in a lack of
 capacity to produce the enzymes that metabolise histamine. In addition, an overgrowth of certain types of bacteria that make histamine from undigested food, leads to a build-up of histamine in the gut, overwhelming the body’s ability to break down the excess histamine. This causes a heightened sensitivity to histamine-containing foods and an increase in symptoms that are commonly associated with allergies. Thus in most cases the underlying cause of histamine intolerance is likely due to existing gut dysbiosis. Therefore rebalancing the gut flora and healing the leaky gut and/or SIBO are the key first step.
capacity to produce the enzymes that metabolise histamine. In addition, an overgrowth of certain types of bacteria that make histamine from undigested food, leads to a build-up of histamine in the gut, overwhelming the body’s ability to break down the excess histamine. This causes a heightened sensitivity to histamine-containing foods and an increase in symptoms that are commonly associated with allergies. Thus in most cases the underlying cause of histamine intolerance is likely due to existing gut dysbiosis. Therefore rebalancing the gut flora and healing the leaky gut and/or SIBO are the key first step. - Secondly, liver function support is of key importance – especially if you seem reacting to almost anything: food, scents, skin products etc. Histamine is also broken down in the liver (by the histamine N-methyltransferase enzyme) so if liver is not functioning well it will impair histamine breakdown. Functional liver tests and/or genetic tests are of value here to get to the root of liver dysfunction.
- Thirdly, good hydration – water regulates histamine secretion and without adequate hydration histamine overload problems are unlikely to resolve. For details on optimal hydration and electrolytes read my posts HERE.
- Addressing methylation problems with testing, supplementation and diet. Testing is required to identify genetic mutations in certain enzymes such as MTHFR gene mutation. Two key variants tested for at present are C677T and A1298C.
- Low histamine diet – a very important part of any natural approach. Adhering to a low-histamine diet for a period of time (or forever for some people) brings fast symptom relief in majority of cases. Sometimes when we start the treatment some particularly sensitive people are not able to tolerate any animal products, and need to follow a plant-based diet to heal the gut and decrease the sensitivity. Fortunately, overtime these individuals will most likely be able to include some animal products in the diet. It’s important to identify specific trigger foods for each individual in order to reduce symptoms rather than indefinitely follow a strict low histamine diet. Low histamine diet leads to increased (improved) DAO levels, likely via its positive effects on the gut.
- Include anti-histamine foods in your diet that decrease inflammation and stabilise mast cells. These include garlic, onions, holy basil, thyme, chamomile, peppermint, ginger, turmeric, apples and pomegranates.
- Low FODMAP diet – for a period of time (up to 3 months and review) to heal the gut and reduce symptoms. Find out more about it FODMAP diet here.
- Eating fresh food as much as possible and avoiding consuming leftovers because the levels of histamine increase as the food ages. This practice has been recommended by Ayurveda for a long time. According to Ayurveda left over food has lost its prana, its vital life force, which results in the formation of ama, or toxic undigested material. This substance clogs up the vital channels of the body, disrupting digestion and ultimately giving rise to everything from fatigue to disease. Since food begins losing prana the moment it’s harvested, it is important to create meals using mostly the freshest ingredients and not to overcook them (7).
Fortunately, after addressing the cause(s) of histamine intolerance most people are able to add some of the histamine containing foods back in without any ill effects. - DAO enzyme supplementation to break down excess histamine, if appropriate. DAO enzyme is produced in the lining of the small and large intestines.
- Addressing adrenal fatigue – which is an inflammatory condition. This could be a complex step depending on the level of adrenal exhaustion present. Check out my detailed post on adrenal fatigue here.
- Addressing any inflammatory conditions present for each individual, as these are a great burden for the body to deal with in addition to high histamine, an inflammatory state.
- Supplementation – here is a broad list of natural antihistamines and other helpful nutrients that help to alleviate histamine intolerance. I choose and recommend 2-4 as needed for a particular client.
- Quercetin – a powerful antihistamine and anti-inflammatory natural compound (16)

- Bromelain – antihistamine, powerful enzyme, works well with quercetin
- Pine bark extract – antihistamine, antioxidant and anti-inflammatory (14)
- Vitamin C – increases histamine degradation and removal (15)
- Vitamin B6 – increases DAO activity (2)
- Herb Holy Basil – has antihistamine and anti-inflammatory properties (8)
- Magnesium – histamine production increases with Mg deficiency (5)
- Pancreatic enzymes – help break down excess histamine in the gut (2)
- Vitamin E – stabilises mast cells thus decreasing histamine production
- Fish oils – highly anti-inflammatory and immune system supporting
- Probiotics containing histamine reducing or histamine neutral strains including Bifidobacterium infantis, Lactobacillus plantarum or soil-based probiotics which tend to be well tolerated by people with histamine excess.
- Quercetin – a powerful antihistamine and anti-inflammatory natural compound (16)
Book a consultation now to discuss your gut symptoms related to histamine intolerance.
Note on antihistamine medications
Antihistamine drugs can be useful as a “rescue remedy” for occasional use, but used daily as a preventative therapy they have adverse effects. Antihistamines act by blocking sites on body cells that would normally act as receptors for histamine. The receptors act as entry-ways into the cell to allow histamine to carry out its function. Antihistamines stop histamine activity by blocking their entrance.
If this blockage is constant, the immune system sees this as a problem and senses that it must be producing inadequate levels of histamine. It therefore increases its production. Consequently, over the long term, there is even more histamine for the enzymes to breakdown and the problem of histamine intolerance becomes even worse (11).
Importance of sleep, rest and stress management in addressing histamine intolerance
Did you know that sleep is one of the most underrated, simple and easy things you CAN do to improve histamine intolerance and start the recovery?
I always discuss and address sleep issues at the start of any natural treatment, including with clients suffering from various forms of gut imbalances. They need to sleep better to gain more energy needed to initiate the body’s healing processes.

Having seen many fantastic outcomes of improved sleep in my practice, I created a short free ‘better sleep’ guide for my clients. The guide comprises key practical tips based on my clinical experience and research, to give you the most important, common sense steps and actions you can do right now to get sounder and more restful sleep tonight.
This FREE sleep guide, in a form of an eBook, will provide you with the key tips and guidance to improve your sleep.
Download your copy of the FREE Sleep Guide here: Top 3 Nutrition tips for better sleep tonight! Key nutrition tips for insomnia plus my top 3 bedtime snacks for deeper and restful sleep
Summary
All who have histamine intolerance of any kind need to take steps to manage it and bring it back under control by means of specific diet and supplementation.
Most foods contain histamine, so we can’t have a histamine free diet like we can have a gluten free diet.
Optimising the gut function, microbiome composition and digestion are the key pillars to resolving histamine intolerance for good. It may be possible to reverse histamine intolerance through gut repair and rebalancing the microbiome alone, even in sensitive people.
As histamine intolerance is currently a fast growing area of research as well as clinical focus, I’ll be adding updates and tips to this post on a regular basis. Please subscribe to my mailing list to keep up to date – look for the subscription box on the right if you’d like to be notified when updates are added.
If you think you may have histamine intolerance, consider posting a message below or booking an appointment with me to discuss your circumstances. At present I’m able to consult with Australia-based clients only.
To book a consultation, either in person or via Zoom click the button below. I also offer a free 15-minute initial discussion to talk about your circumstances and how I can help.
I look forward to connecting with you and to helping you to feel healthier and happier soon!
Please note that the above material is for informational and educational purposes only and is not intended as a substitute for medical advice, diagnosis, or treatment. Consult with your health practitioner or doctor for advice specific to your circumstances.
Best of Health![]()
Joanna Sochan
Wholistic Health and Lifestyle Therapist
Natural and Lifestyle Therapies for Abundant Health and Wellbeing
References
Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr 2007;85:1185-1196
Essential Ayurveda: What It Is and What It Can Do for You. http://www.yogajournal.com/article/balance/lifeless-leftovers/
http://www.histamineintolerance.org.uk/about/the-food-diary/the-food-list
10. Joneja JMV, Carmona Silva C. Outcome of a histamine-restricted diet based on chart audit. Journal of Nutritional and Environmental Medicine 2001;11(4):249-262
11. Joneja JM. Histamine intolerance. It feels like allergy; It looks like allergy; but it’s not an allergy. Foods Matter Newsletter March 2010
http://www.judytsafrirmd.com/histamine-intolerance-gaps-and-low-carb/
Iravani, S., Zolfaghari, B., PhD, Pharmaceutical and nutraceutical effects of Pinus pinaster bark extract
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3203267/
Rock, C.L., PhD, RD; Jacob, R.A., PhD; Bowen, P.E., Phd, RD, Update on the Biological Characteristics of the Antioxidant Micronutrients Vitamin C, Vitamin E, and the Carotenoids
Kang JH, Chang SY, Jang HJ, Cho JM, Kim DB, Lee SS, Ko SH, Park YM, Needs PW, Jo YH, Kim MJ. Quercetin-induced upregulation of human GCLC gene is mediated by cis-regulatory element for early growth response protein-1 (EGR1) in INS-1 beta-cells. J Cell Biochem. 2009 October; http://www.ncbi.nlm.nih.gov/pubmed/19798679
Tsimmerman, Y. S. “Study of intestinal dysbiosis (“dysbacteriosis”): state of problem and new trends.” Herald of Pancreatic Club 45.4 (2019): 44-53. https://vkp.org.ua/index.php/journal/article/view/177
Folkerts, Jelle, et al. “Effect of dietary fiber and metabolites on mast cell activation and mast cell-associated diseases.” Frontiers in immunology 9 (2018): 1067. https://www.frontiersin.org/articles/10.3389/fimmu.2018.01067/full
Kakolyri, Maria, et al. “Increased Basal Blood Histamine Levels in Patients with Self-Reported Hypersensitivity to Non-Steroidal Anti-Inflammatory Drugs.” International archives of allergy and immunology (2019): 1-7. https://www.karger.com/Article/Abstract/503968
Photo credit: Shutterstock
Additional resources
- What is leaky gut?
- Secretory immunoglobulin A (sIgA) for healthy gut, digestion and immunity
- Parasite treatment considerations: Blastocystis hominis and Dientamoeba fragilis
- Adrenal fatigue treatment: The Kalish Method in Australia
- Holy basil – a key herb for stress, anxiety, depression and fatigue
- Top nutrition tips for insomnia and interrupted sleep
Disclaimer: The above material is for informational and educational purposes only. It should not be used to self-diagnose and it is not a substitute for a medical advice, diagnosis, treatment, prescription or recommendation. All viewers of this content, especially those taking prescription or over-the-counter medications, should not make any changes in their health regimen or diet before first consulting a doctor or other qualified health provider with any questions they may have regarding a medical condition or their particular circumstances.

Joanna Sochan is a Natural Therapist and founder of Naturimedica Holistic Wellcare. She has a passion for helping clients transform their lives by becoming healthy and well naturally. Joanna has 12+ years experience in clinical practice and has special interest in solving complex cases, gut health, food sensitivities, hormone imbalances, autoimmune disorders and weight loss. She helps clients individually (mostly online) Australia-wide and also offers online therapeutic programs, eCourses and self-help books. View full bio.
 Print This Post
Print This Post 


I have been having histamine intolerance manifested in a hives breakout every 40-48 hrs for almost 2 years. Sadly I have been on a antihistamine for about same period. I recently got diagnosed with dysbiosis occasioned by low stomach acid and low secretory IgA. I also have increased levels of H pylori. This has all made it clear to do a gut reset, especially following the triple antibiotic therapy which was unsuccessful in ridding the H pylori.
I have been following the gut reset protocol from a naturopath/functional doctor. The confusion though is on the recommendation to take fermented foods. Considering fermented foods are high histamine; how does this conflict get managed ?
That’s right, the hives indicate excess histamine production coming from the dysbiotic bacteria in the gut. You likely have too many bacteria producing histamine so doing a gut reset is the way to go. Personally, I encourage clients to have fermented foods in quantities that don’t trigger symptoms.
I find that sensitivity to so called high histamine foods is an individual reaction, and many people can actually tolerate many high histamine foods, including fermented foods. So it’s worth testing if you’re one of them.
Secondly, fermented foods are high in beneficial bacteria needed to rebalance the microbiome and will relatively quickly affect the levels of bacteria towards better balance and as such decrease the histamine producing bacteria.
Food preparation and storage also make a big difference to histamine levels in food.
Meat left in the fridge for more than 1 day will increase histamine content, after 2-4 days histamine will be high. Freezing Meat/ stock in daily portions shortly after cooking will stop the histamine formation.
On the contrary, more mature sauerkraut and beetroot kvass have less histamine over time. Buy more and keep them in the fridge, taking what’s needed every day.
Hope this helps.
Joanna
I believe I may have a histermine intolerance
Hi Francine
I’ll get in touch with you shortly.
Wow, what an informational article. Histamine intolerance explains a lot of my issues and one day I will try and get the lab work done as I believe I have a gene or methylation problem since I have had issues since birth. I do eat a lot of the vegetables as I try and eat fiber and want to improve my immune system. I have a drive and passion to help myself and others to be healthy and get to the root of problems instead of going on meds just to manage something so I keep researching as God leads me. My husband says I am not trusting God and I do and He has diminished a lot of the problems I had but I still keep praying He will tell me what is wrong with me as I am irritable because of issues.. It took a few years of getting rid of candida, changing my diet, and trying to restore gut health as I had reflux really bad. I went off all allergy meds, reflux meds, miagraine meds, but til took Sudafed for the vasomotor rhinitis as I still can’t handle smells from smoke, perfumes or chemicals, Nsaids, ( the complete hysterectomy for the endometriosis took away all the pain I had.) Turns out I had low stomach acid as I knew meats didn’t sit with me well. So I did HCL and enzymes which helped a lot. I had a lot of pain from car wrecks not my fault which caused fibromyalgia and still have nerve damage in my neck and around the lung area so I make a turmeric, ginger, black pepper drink every morning to help with that inflammation. I still have the bloating and sometimes gas after eating plus the annoying nasal problems, itchy ears in the am even though the mucus isn’t like it used to be as I quit drinking milk. I was so blessed not to have had a cold or bronchitis last winter. I still can’t figure out what to do about the vasomotor rhinitis as I am snoring so much at night now as I can’t breathe. I asked my husband if I stopped breathing and he said no- I just make whistling and other noises that bother him. That is what started me researching again what I can do as I can’t go to a naturpath or functional dr yet. I don’t have insomnia anymore as I am out after a few minutes and can sleep a good five to six hours or so til my husband wakes me up then I am up for a while. I quit drinking liquids after 4pm so I can sleep at night as I still have interstitual cystitis. Sorry this is so long but it looks like either I have a low stomach acid issue, low B6 and probably B12 now or lack of the DAO. Thank you. .
You’re welcome! I suggest you find an experienced practitioner to work through the further potential deficiencies you may need to deal with.
Thanks for your article Joanna, and I really enjoyed and appreciated my initial free consultation with you.
Firstly I want to add a symptom that is missing from your list but was on another list and that was really helpful in me recognising HI as my issue, and that is having a dry cough. Also, I often experience my ‘tachycardia’ as less of a racing and more like a deepening of the heart-beat, as if my heart is having to work REALLY hard to pump the blood (just in case that’s useful to anyone).
Since speaking with you, about a month ago, a combination of watching something inspiring and putting some observations together, I started eating one meal a day (more or less), focussing on lunch. My most impacting symptoms have been tachycardia and related insomnia. Eating one meal a day has not only been a major and exciting ‘life hack’ but it has revolutionised my insomnia and I’m feeling like a ‘normal’ more or less healthy person! Simply, eating one meal a day has significantly reduced my overall histamine load (less food going in for my body to process), as well as eating in the middle of the day so my body has a chance to work through any histamine excesses before bed-time. Taking DAO has been very helpful, and of course doing my best to reduce my histamine intake (sometimes tricky), and these efforts are not at all comparable to the profound shift in symptoms from simply not consuming as much food. I also cut C-zine anti-histamine tablets in to quarters and so take that sparingly before bed or during the night if I’ve been a ‘naughty girl’ (consumed too much histamine during the day, or eaten low histamine foods in the evening) and this has also really helped, while recognising it’s not a long-term strategy, it’s helped to get my life back in the short term and hopefully setting myself up better for other more substantial and foundational changes.
I understand that for many folks eating only one meal a day is a difficult step to take.. There’s been things I’ve been engaging with for a little while now that has supported me to be able to take this step. I’m also mostly dependent on animal proteins and fats, which again I find takes a very big immune-managing load off my liver and is when I get the best results. However if you have folks who are really looking for results, this may be a useful strategy alongside your other guidance and support :)
Hi Joanna
Interesting article it sounds like I have histamine intolerance. I think it all started 8 years ago when I had estrogen dominance and at the same time I had very bad vertigo and weight gain. At the time I went to a doctor who prescribed bio identical hormones (peri menapause) and things got much worse.
Since then I have really chronic vertigo a day during hay fever season this year being the worse. I was bed ridden for weeks and had to have fluid drained from my ears and grommets put in. And I’m also going to another specialist to have my nasal and head drained from a
Very bad sines problem which has left doctors concussed why it’s been so bad.. Im only dubtuining because they out me on endep which I hate to help me. But this is only a bandaid.
I have notice that since I had vertigo I also had continuous weight gain and sugar cravings getting worse. When I have a vertigo attack I notice if I slightly over eat in the evenings
My vertigo instantly gets worse it’s very strange it’s like the bucket over fills.
I’ve had many test and have low seratonin high metabolise colestrol, low zinc, high copper and very low b’s. So my naturopath has asked me to do compressive stool test. Which I will get result on Tuesday.
I’ve tried everything from low carb diet lost weight first 2 weeks then gained again. I also have high reverse t3. Hopefully this latest stool test will give me answers.
Love to hear your thoughts.
Sorry for the essay
Thank you for sharing your experience. Doing the comprehensive stool testing sounds like a very good idea at this stage as the gut function needs to be assessed to gauge your digestive capacities (stomach acid, protein, fat and carb digestion)as well as bacterial balance, and exclude any parasites or harmful bacteria (PCR type testing is important here). Toxins produced by them can be a factor here.
I would also suggest to examine the lymphatic system in relation to vertigo and excess water in the ear. Addressing the nutritional deficiencies you mentioned – low zinc, high copper, low B vitamins etc would also be a priority.
Thank you very much Amie for sharing your experience and tips that helped you.
I think eating one meal per day is a grea4 strategy for histamine excess for the reasons you mentioned.
I’m very glad you’re feeling better, you might’ve inspired other people who’ll read this by taking the time to post!
Thank you again.
Hello Joanna,
Thank you for your article. I’ve had histamine intolerance since I was a child. When I consume something high in histamine my stomach bloats, I retain water, have constipation, and will experience my nose/hands flushing and dilated veins. I have observed that the same thing happens to me when I consume vitamin C…. however vitamin C is known to be an antihistamine. I realize now that I get the same reaction from foods that have a low PH. Taking PH buffers like calcium carbonate will reduce/ prevent the reaction from occurring. I react to spinach, chocolate, citrus fruits, bell peppers, spices, many herbs, anything fermented especially alcohol. I know all of these items are high in histamine. They are all also low on the PH scale. I think the PH of foods efffects how the body releases histamine. I am worried about taking the bifidobacterium strain probiotic even being histamine degrading because the low PH the bacteria produces…. I am afraid I would still have a reaction to it. I would love to schedule an appointment with you to discuss this matter more however I am located in the United States.
Hi Nicole
Thank you for your comment. I’ll respond to you via email.
Okay,
Thank you!
Hello Joanna,
Thanks for the really insightful article. The last year I am suffering with gut issues, insomnia and really fast heart rate..especially when i stand up. Lately I developed as well intolerances to foods I could eat normally previously. Few months ago doctor perscribed hydrocortisone and I felt better 9nly for a month or so. Now the situation is even worst.. after food i know i will have diarrhea, even faster heart rate , bloating and intestinal discomfort. Is this at all related to histamines or dysbiosis?
Thanks
Hi George
Food intolerances are pretty sure pointers to gut imbalances such as inflammation, leaky gut, good/bad bacteria imbalances (microbiome imbalances), gut parasites and other symptoms such as diarrhoea and bloating. In such cases it’s not the foods that are the problem, it’s most likely the gut that needs urgent attention. I suggest you consider a comprehensive stool test such as Genova GI Effects or Diagnostic Solutions GI Map and working with a practitioner who can interpret them and develop a treatment plan for you.
Hope you’ll get better soon.
Hi Joanna
Your articles are really helpful. I think I have histamine intolerance which has just started just a month ago. I have been experiencing itching,in fact severe one, on my skin for the past few weeks whenever I’m emotional, stressed and when exposed to sun or heat. I also hardly sleep and I do have nosal congestion. I have been doing research on the causes and I realized that it might have been caused by the intake of peanut because I don’t used to eat peanuts but when I started taking it, this problem started. My question is, I stopped taking peanut since I realized this connection between the two but I’m still suffering. what am I suppose to do to get rid or reduce the symptoms?
Yes, I might be having some gut issues because my digestion doesn’t work as well as it used to and I think I will look into that with my doctor but do you have more to add in order to help me get out of this condition? I’m 23 and still a student and it’s actually hindering my work at school
Mike
Hi Mike
Thank you for your enquiry. I suggest you strictly follow the low histamine diet for 2-3 weeks to see if too much histamine is the culprit here. If your symptoms are gone or significantly diminished, this means you’ll need to work with your doctor on reducing histamine using the methods described in my article to deal with histamine intolerance. If not, other investigations need to be done to find the cause of your current symptoms e.g. food intolerance testing.
In April was diagnosed idiopathic angioedema. Most recent lip swell happened overnight after an anxiety “attack”- something new to me. I am 58 and have had a very stressful life situation for the last year and a half , I eat mostly low carb , take no medications, supplement under guidance iof my PC dr. Something is out of whack!! Allergist says take more Zyrtec, PC did blood test for food and environmental allergies with small indications of dust, animals, nettle and elm. My fatigue level is high. I am researching stress-‘adrenal fatigue and HI. Your article is very informative ! Do you have thoughts on next steps besides Naturopath.
Thank you!
–
Sounds like quite a few body systems are not performing at a good level at present and you need help with determining treatment priorities. I DO suggest you see an experienced naturopath or nutritionist who is well versed in treating gut imbalances because a big picture view approach is needed in such cases. Otherwise a functional medicine doctor with gut health focus would also be a good start.
I enjoyed reading your article on histamine intolerance. I am curious how essential oils play in this. In other words if clove, cinnamon and nutmeg spices in food add to a histamine overload, what would clove, cinnamon and nutmeg essential oils do? Would you have the same reaction? Also, what if you applied them topically , or aromatically, and not take them internally? My son has a problem with histamine and we use EO’s. Are we adding fuel to the fire?
I’m glad you enjoyed reading my blog on histamine intolerance:)
It’s important to remember that each of us reacts differently to foods, herbs and essential oils as well. Lists of foods good or bad for a certain condition are guides only and they need to be tested for each individual to see any reactions. So essential oils could be beneficial for one person or detrimental for another.
Essential oils are very concentrated plant extract that are highly potent. If ever ingested internally, it needs to be supervised by a trained person well-versed in applications and safe doses, especially for children. Otherwise significant damage can be done, especially to the digestive system lining throughout.
Reputable supplements containing essential oils are much safer as the recommended doses are most likely researched and validated clinically.
Topical applications of essential oils are safer providing the oils are diluted in a carrier oil such as almond oil.
Supplements with essential oils are used in antimicrobial formulations to eliminate ‘bad’ gut bacteria but they also affect the ‘good’ ones. So it’s a cleanse type of treatment to start with followed by gut re-population with beneficial bacteria and gut repair nutrients.
I also think I have an intolerance to histermine.
My skin feel like it’s fighting it’s self.i mean any foreign Hair or flea or mosquito I break out in hives then I scratch until it bleeds to get some relief. I have been suffering for over 35 years.
Not sure what to do next!
Yes, it sounds like histamine sensitivity. Did you have this checked by a naturopath?
Hi Joanna,
Thank you for the great article !
Are you still in Sydney ? I have been suffering from a similar condition for more than 1 year now, and would like to book an appointment to discuss further. Please let me know if its possible..
Thanks & Regards,
Sahar
Hi Sahar
Thank you for your comment!
Yes, I’m in the Sydney clinic on Mondays and Wednesdays, also doing online consultations on Thursdays & Fridays. Call me or send me an email re booking when you’re ready.
Hi Joanna,I just loved your article. I have chronic urticaria and I am on xolair injection for months now. Recently my son is also experiencing histamine intolerance. He was diagnosed for allergy to almost all food now. Hard to feed him and unable to see him suffer, I feel so guilty that I have passed on my gene to him. He is only 4 and the allergies interferes his life everyday with diarhea. If there is a cure for him, I will be so grateful to you. Thank you.
Hi Rupa
I’m glad this information is of help to you. Even genetic conditions can be improved by adjusting the internal and external environment/ factors. His digestive system/gut is likely damaged with imbalances in gut flora and perhaps parasites as well. I suggest you find a naturopath/ doctor who understands how to identify, assess and then correct these imbalances with supplements, right foods and gentle detox. Don’t despair, there is hope – look for answers until you find them!
All the best <3
Just recently found out my gallbladder is only working at 6 percent. I started extreme itching, no hives or bumps. Severe dematsis. Itchy red eyes, some discharge from eyes. Could gallbladder cause histamine issues? First allergy test was negative. Have not taken food test. Dermatologist thinks something internal.
Gallbladder that has diminished capacity changes how the digestion works, especially digestion of fats is impacted as bile is needed for it plus for absorption of fat soluble vitamins (A, E, D, K – people with gallbladder disorders are usually deficient in these). Lack of bile causes imbalances of bacteria in the gut potentially leading to sensitivities and intolerances, including contributing to histamine intolerance, depending on a person.
I suggest liver support in this case (foods and herbs) and supplementing with ox bile / digestive enzymes to gauge to what degree the gallbladder is causing your symptoms. I would also check for vitamin deficiencies (as stated above) especially vitamin A – see my article on vit A here: http://naturimedica.com/?s=vitamin+a
No, I’m afraid the probiotic I was taking was making my histamines react. I went to just chicken and rice and my face flushes after my morning meal only. This has been since yesterday.
After going on an elimination diet of just chicken cooked an eaten immediately from frozen, rice, oatmeal (plain with water only) and broccoli and zuchini cooked fresh. I still itch a little on my chin and cheeks. Is this normal? I have only been at it a week. I’m wondering if I can’t have the things I’m eating. I don’t get the burning cheeks or ear pain and dizziness anymore or the stomach cramping. Not sure if I’m doing something wrong.
It takes time for the symptoms to settle. Are you doing any gut repair/ support whilst on this elimination diet?
I have had gut issues for over ten years. I’ve been on so many different natural treatments, probiotics, have had probably 20 different stool tests in that time. At one point I developed C diff after being treated with antibiotics for kidney stones while in the hospital. Long story short, I have a bad bacterial imbalance in my gut which I have been trying to rectify for years. Believe me, I have seen all kinds of doctors for this problem. My main question is this: I think my histamine issues have gotten so bad that I now have terrible episodes of coughing/choking and coughing up sputum. It feels like my throat is closing up and my nose and eyes drip like faucets. This happened today in the grocery store and because I couldn’t catch my breath, I had to motion for the manager to get some water. It is now 5 hours later and I still cannot speak without coughing.
I think I am at the stage of carrying an Epipen so that I don’t go into anaphylactic shock. Has anyone here ever gone this route? I continue to work on my “allergy and histamine issues”. The sad thing is that I can only eat chicken, almonds, butter and homemade chicken soup. I cannot eat any: wheat/grains, vegetables, fruits, dairy, eggs, alcohol, spices, etc. So my diet is already severely limited. It does no good for people to tell me to go on the SCD or GAPS, because most of the foods are not tolerated by me. I am at my wits end with this.
I am currently looking for a probiotic with the strains which you mention, but they are difficult to find.
thanks
Thank you for your comment. Where are yo based? Wagne’sr Probiotica has many strains I mentioned and can be bought over the counter. There are also other “practioner only” probiotics I prescribe (I’m based in Australia).
Your symptoms point to a damaged gut wall, leaky gut and bacterial imbalance (such as SIBO). Probiotics help but are only one part of the overall treatment needed. here.
Is it possible to buy DAO sin in Australia please
My ganddaughter is on a gut protocol with high histamine and the naturopath said to take it
She usually prescribe seeking health brand but can’t get it
Thank you
I haven’t come across DAO enzyme probiotics that are made/sold in Australia, I’m afraid. let me know if you find a supplier here, please!
Years ago I had a bug bite that ended up infected with staph causing cellulitis and a whole body itchy hive and swelling reaction they called an “id reaction”. Since then my skin is incredibly sensitive to lavendar which did not bother me before. Then I started getting random itchy welts without any known triggers…often while warm. Finally it would get way worse when sick with a simple cold. I also noticed my reactions to known allergens s would result in excessive phlegm and a croupy cough. I did a low histamine whole food diet x 5 weeks and added foods back without issue. Also taking probiotics and but D3. Magnesium when I remember. Now I have a virus again and had to take benadryl because it’s so bad. Suggestions? If I see a Dr who can help me? Also started with low progesterone symptoms past few years which must b related somehow. Not convinced the diet helped but will try whatever.
I suggest you look into supporting your immune system to start with as bacterial and viral infections, as well as food sensitivities indicate a malfunctioning immune system.
Allergies are caused by a faulty response of the immune system. It reacts to allergens – substances that the body views as threat and attacks. The symptoms of the allergy are an expression of this misguided defense mechanism.
Many scientists are pushing a theory that focuses on the increased incidence of allergies in current populations. According to these scientists, excessive cleanliness leads to bacterial imbalances and an over-active immune system.
Thank you for your comment Margo. Yes, it’s an interesting point of view which also makes sense to me from a clinical perspective. As I’m sure you are aware, most of the immune system is actually located in the gut to deal with any ‘dangers’ coming from the environment via what we ingest or are exposed to. Having a leaky gut causes bigger food particles, which are supposed to stay within the gut walls, to “leak” into the blood where they are spotted by the immune system, treated as foreign and attacked/ dealt with in a number of ways. This contributes to the development of food and other allergies – the mechanisms are known and can be found online e.g. https://ucfa.nl/food-allergy/mechanisms/
Hi Joanna I just found this post! Can you please tell me if the Bifidobacterium Breve strain /category of probiotic lowers histamines?
I was taking LB coagulans, having read that it lowered histamine and then I had a severe attack – my skin becomes inflamed, largely in my scalp. I later read that Coagulans RAISES histamines, so really upset about that misinformation – I am really careful about my sources so felt duped! I’m thinking of trying Breve as its in a combo with Longum and Infantis that looks good for me, but wanted to find out if you can confirm that Breve lowers histamines?
I also have low hormones – all of them – and I had been raising my progesterone at the same time, so I wasn’t sure if it was the comparatively lowered estrogen and/or raised histamines that was causing the issues. Anyway my histamines went crazy. I understand from one of the hundreds of papers I’ve read on the complex arena of histamine that histamines rise in order to try and raise estrogen too! So it may well have been both. I don’t detox histamines or other amines well (MTHFR mutation) so for me, one little mistake is disasterous. The wrong food is bad enough – the wrong supplement is a nightmare.
I’ve had so many naturopaths who have made me ill with supplements that were dangerous for me, even a multi! It’s great to read a post from a naturopath who is up to date with this very complex area :) Thank you
Hi Christina
Yes, as far as I know Bifidobacterium breve is anti-inflammatory (together with Bifidobacterium infants and Bifidobacterium longum) and it shouln’t raise histamine levels. For example, the ProBiota Bifido supplement (from Dr Ben Lynch in the US) contains the beneficial/neutral probiotic strains that help with excess histamine. Here’s the link https://www.seekinghealth.com/probiota-bifido-60-capsules
Thank you for your comment! I have now updated the probiotic section of my article to make it clearer which strains are OK/neutral for histamine excess.
Hi Joanna,
My wife has been suffering from histamine intolerance and we have begun a low histamine diet. Could you explain why chili powder is bad (not sure if this is the blend or pure ground chilis)? Hot peppers are something I have also seen on multiple lists as being bad, but bell peppers have been listed as good. Any thoughts on why they would be high histamine. Thank you for your time and the article.
Hi Nathan
I’m afraid I don’t know the answer to your question. As far as I understand there is no “perfect” list of foods that trigger/ enhance histamine release. Many foods that are included on those lists as the triggers can be eaten by some people with known histamine intolerance with no symptoms, others are unable to tolerate some of the OK foods. We are all different and you’d need to experiment with any foods you’d like to include in your diet to see if they trigger any high histamine symptoms you have. I recommend an elimination diet type of approach to identify your wife’s trigger/ OK foods.
Hi Joanna,,
I’ve had HIT for years, getting worse, with severe cramps etc etc. Shortly before Christmas 2016, I started magnesium oil spray and Epsom salts as I can’t tolerate oral magnesium. It solved lots of problems: no more cramps, a lot more energy, far better sleep, relaxation, more variety in diet and more. All that in less than 4 weeks! I still have some histamine problems but maybe that can be fixed as well over time. At least I can eat more anti-histamine foods and can get rid of my anti-histamine medication.
I particularly like your list of HIT supplementation. Red cherries and cherry juice are supposed to be excellent as well.
Kind regards, Bridget
Hi Bridget
Thank you very much for sharing your experience with magnesium oil spray and Epsom salts as sources of magnesium that worked for you. Very interesting and good to know for others who read this post looking for possible solutions. Please keep me posted on how you’re going after adding other options such as red cherries or cherry juice.
Hi :) great article and links. Thank you.
Just curious when u say soil based probiotics? What do u mean by this? Are there brands that produce these? Cheers ;)
You’re welcome! By soil based bactetia I mean beneficial probiotic bacteria that live in the soil. These are relatively new probiotic strains that are added to some probiotic formulations. I mean the strains are not new per se as they have been present in soil/dirt since forever and we’ve been exposed to them since birth but to a lesser degree for the last few decades since the food is sprayed and washed in chemical mixes before it gets to us.
I suggest you look on iHetb.com for product suggestions as I don’t use soil based probiotic at present but am looking for good brands as well!
Dear Joanna
Thank you for your helpful article!
I still have questions about that topic. In connection with mast cells that are located in the gut, the lungs, the skin, the mouth… How mast cells react if there are bacteria in the gut that activates those mast cells? I know for e.g. that E.Coli can produce huge amounts of histamine by themselves and also by activating the mast cells. But is this just going on locally in the gut? Or can the mast cell activation / or histamine release affect then the whole body?
I ask you this because I have SIBO.
I guess, I generally have high histamine in my body. If I am stressed, if I am exposed to the sun or if I am emotional I get a very quick histamine reaction. But I do not react on high histamine foods. Therefore I think the mast cells are my problem and not low DAO.
But I do not have just gut histamine symptoms. My tongue swells up a bit, I am hyperventilating (not severe but for many hours or even days) and I have angiooedema in my fingers.
So, is it possible that the mast cell activation via bacteria in the gut affects the whole body, also the lungs?
And is it possible that this overall activation is made worse if exposed to some other triggers like the sun or stress?
Or is it more likely that I have kind of mast cell disorder AND bacteria, both producing histamine?
Thank you for sharing your knowledge
Nicca
Hi Joanna,
I had anaphylaxis twice within 6 months time in 2016. First in June and then in November. Both times I was asked by general physicist to take corticosteroid and Allegra along with Rantac for 20 days. But the exact reason for the allergic reaction has not been found yet. Initially it was thought it was milk allergy after the June incident. But after the November incident, I consulted an allergy specialist who thinks it may not be related to food allergy and something related to respiratory issues. I forgot to tell my doctor that I was on and off antibiotic tablets – Banocide Forte for 2 – 3 months in 2014 and again in 2015. Would this be the culprit in high histamines in my body?
I would like to mention that I had anaphylaxis in June within 30 minutes after eating a heavy snack that included cream buns, vegetable puff and tea (with milk). Then in November, I had anaphylaxis within 30 mins of eating Rotis (Indian Dish made from wheat flour).
Can you please share your views on what could be the possible item triggering causing anaphylaxis in me? I am really frightened as I have been told that anything may happen to me anytime and I am in a life threatening situation.
Thanks!
Thank you for your comment. I’m afraid I can’t give treatment advice online no matter the condition. Keep searching for the answers as to the cause of your reactions and I suggest you look for skilled practitioners such a gut specialist or immunologist that you can see in person.
I live on anti hystamines as I seem to react to everything ! I have had allergy tests and I am allergic to coal tar and two chemicals which I no longer have anything with these in. my eyes are permanently ichy red and runny and I have raised Ana levels. I have been signed off from the dermatologist but I am still under rhumatologist. I do not have arthritis but remain under him as I have aching joints particularly hips knees and shoulder. Is there a possibility that I am histamine intolerant?
As I mentioned in my article, gut health and digestion are closely related to histamine intolerance, among many other problems. I suggest you look into going on a strict low histamine diet for a month to see if your symptoms improve. If yes, this is a good indicator that you likely have histamine sensitivity/ intolerance. Increased ANA levels indicate a presence of an autoimmnue condition so you’ll need to look at it as well with your health practitioner.
Hi. I’ve been having a severe sinuses allergy for more than two years and living on aerius and telfast and getting worst.
I started xolair recently and got a bit better.
Is it histamine intolerance and do u think I might be able to cure it?
Hi there!
From my experience sinus issues are very often related to gut health and indicate imbalances there. It could be histamine intolerance, problems with absorption of nutrients or gut wall integrity problems (leaky gut) which are associated with allergies of all sorts, to name a few. I suggest you follow the low histamine diet for 3-4 weeks to see if this improves your symptoms. If yes, you may have histamine intolerance and if not, look at the other aspects of gut health to focus on.
Hi Joanna,
Very interesting reading this post. I’ve had SIBO in the last 8 months but successfully got rid of it through treatment from a naturopath / functional medicine practitioner and strict diet in England, where I’m from. I’ve suffered with hayfever and eczema my whole life, at the time of the SIBO diagnosis my eczema was appallingly bad. It is very bad at the moment, I think not helped by the pollen levels, and a naturopath I have been seeing here in Sydney recommended a histidine tablet for the hayfever. I took one and I felt that it made my symptoms much worse. I’m actually studying to become a naturopath myself at the moment and I’ve just got to a part in my course about histidine. But everything I read makes me think that taking a supplement of histidine would surely make my eczema worse ? I don’t quite understand why my practitioner suggested it. Many thanks! Grace
Hi Joanna
Thanks for your answer. I am taking an Austrian brand called (DAOSIN made by Sciotec) which seem to work best for me . Also Histame is good but the production was stopped for some reason. Other brands were not so effective. Do you think that most doctors understand the parameters of such stool test? Thanks a lot for your efforts .
I’m afraid not many doctors know how to interpret the CDSA results. You’ll need to look for a naturopath or functional doctor to have them interpreted and appropriate actions taken re histamine intolerance.
Hi Joanna
It took me 5 years to understand what was causing my headache and stomach cramps . Most doctors i visited related it to IBS. By researching i have suspected that i have histamine intolerance . My suspicion was confirmed when 95% of my problems disappeared after i started to take DAO supplement before food. I am a different person now. The question is : do i have a gut issue even if the symptons disappeared? and how long can i keep taking the supplement? by the way i also lot wight during this problem but my wight is fixed now and i am trying to bring it up a little .
P.S. i have done a medical check to find out the causes of wight reduction but Drs didn’t find anything wrong .
Hi there
I suggest you have the gut function test called complete digestive stool analysis to gauge the state of your gut including how well you digest proteins, fats and carbohydrates; and to check the gut flora status/ balance or otherwise. Taking the DAO enzyme is helping for now but not correcting the histamine issue so attending to your gut health and structural integrity would be dealing with the cause of histamine intolerance.
Could you please tell me what DAO supplement (brand) are you currently taking, please?
All the best
Joanna
Hi Joanna,
Thank you for your posting. I found it very useful. I am a bit confused regarding the section on histamine medication and does that include supplementation? Should a person not take natural antihistamine supplements for a long period of time?
I have just started taking medication for a condition that I have and it has increased the level of histamine produced by my body. It impacts my life as I get a runny nose so I am looking for natural and safe ways to reduced histamine release and I am hoping to take quercetin and bromelain. But, after reading your article, I will include magnesium.
I will also look at improving the health of my gut as it may be a contributor.
Any further suggestions will be much appreciated.
Hi Rose
Natural histamine supplements are generally safer and can be taken for longer periods of time but the aim is always to reduce/ stop any medications/ supplements as soon as possible and let the body to regulate its functions.
Re your medications and taking natural supplements – please make sure that there are no contraindications to taking natural supplements together with the drugs. Also, start taking one supplement at the time (quercetin and bromelain should be fine to take together) for a few weeks and then add magnesium to see any difference either way.
Starting with improving your gut function is going to be your best strategy to address this problem long-term. I’m afraid there are no shortcuts here!
All the best
Joanna
Hello Robert
From your brief description, I suggest you consider doing a comprehensive gut healing work with a naturopath or a functional medicine practitioner near you who understand how to use supplements and foods to repair the gut wall and improve/ restore the digestive function. This approach will help with eliminating/ improving any food sensitivities and/or allergies long-term. Until your gut function is improved it’s likely you’ll keep reacting to many foods (it’s often hard to tell which ones) and will have histamine intolerance symptoms.
All the best
Joanna
Hi Joanna,
i am glad to find this article on internet.
As i had ulcers four years ago and was prescribed with Nexium 500mg tablets for 12 months. Now i have no problem with ulcers, but while i was on medication i started to have rash and very itchy skin. Skin Specialist prescribed me C-zine an anti allergy medicine. i am having C-Zine every day.
Now i think, i have histamine intolerance. My nose always blocked and if i have any alcoholic drink. i have allergic reactions like runny nose, difficulty breathing, itchy skin and rash. After having Vitamin C and C-zine, it gets better. i get flu and cold almost after every 2 weeks now.
just want to know, what do you suggest, i should have to make my condition better. Any medication or foods will help.
Thanks
Thank you for your post. I suggest you follow the low histamine diet as outlined in my article for a month or so to see if this makes a difference. However, the most important thing to do is to look into your gut health (wall integrity and digestion function) and remedy any deficiencies or issues. This will greatly help with any sensitivity or allergic reactions you have.
Hi I greatly enjoyed your article. I have histamine issues as well as candida. I’m a couple months in at trying to heal this and am seeing improvements. I still have reoccurring issues with oral thrush and angioedema in my lips. I see the most results with the low histamine diet but find it hard to follow. What foods can I eat…I feel very limited. Thanks.
Holly
I’m glad you found my article useful for you, thanks for reading!
As I say in my article, the key to reducing/ eliminating histamine sensitivity is to treat the gut by the appropriate diet and by taking specific supplements that will help to repair the gut wall and re-balance the gut flora. Once there is more beneficial bacteria in the gut they will keep the problematic ones under control, including histamine producing species.
Yes, the low histamine diet is difficult to follow and limited. I suggest you pursue the big picture approach here and address the likely cause of your symptoms – the gut function, including gut wall integrity and the ability to digest proteins, carbs and fats to get the most nutrients from your food. There is no way around it from my experience, it’ll help you with both histamine intolerance and candida. You need to find a natural medicine practitioner to work with to address both issues. I often say to my patients: food is NOT the issue, your gut function is!
Hi. Thanks for your input. I followed your link to see if that diet is something i could try but there was nothing in the lnk that said what tne protocol was. There was another link embedded in that one and when i followed it , it was simply an advert to buy the book with not even a summary of what the proltocol was. Incidentally , in my case there is no Psychology (the P in GAPS) in the mix, so what would be left is not GAPS but simply is an argument for dysbiosis, which these days is quite popular for everything that ails. . Been there. Hope you post this reply.
Hi. Thank you for very thorough histamine post. I have reacted badly to aged foods, all on your list, for a couple of decades, but i always thought the culprit was tyramine rather than histamine. They are both amines of course tho tyramine broken down by MAO rather than DAO. Is there any way to detrmine which it is
This may be relevent for me: i seem to have developed a milk allergy, not lactose intolerance. A drop of any dairy gives me diarrhea for 3 days. In retrospect, could be a lifelong problem solince unexplained chronic diarrhea in infancy and early childhood.
I seem tho to be a quiring all sorts of allergies to foods- coconut for exampke. Certain spices seem to give autonomic nervous system reactions – mint and anise. (Also have clove allergy). Lots of foods give ne diarrhea now, tho nothing as bad as the dairy. (Even cooked berries, cooked zichinibetc).
For testing, on a CBC, my eoisonophils are low- below normal (not was on transderval progesterone)- does low histamine rule out a histamine intolerance?
On comphrensive stool testing with doctors data, i have an ansense of lactobaccilus. Since im off all dairy , i was not too surprised by this. The one time i tried probiotics i had such a bad reaction am reluctant to try again. I had a 1/4th of a teaspoon of the juice from bubbas raw sauerkraut. Like with my dairy reaction, was in bathroom for three days.
The other abnormal finding was greatly increased secretory IgA. This suggests up regukated immune reaction, but that could mean anything from parasite to allergy. So far all parasite tests negative. Pancreatic enzymes fine
I dio have chrinic autoimmune illnesses so adrenal fatigue makes sense. So far cortisol testing has been in normal ramge but its on the low side for early am and on the high side for evening- suggesting non optinal diurnal functioning. But taking steroids is not something that i want to do
Final piece of puzzle i will mention is ive had dermographia since age 11,
By the way end result of all of this for me is i am too thin and cannot gain weight. Used to gain weight with ice cream but of couse cant have dairy now) I should add that nearly every “diet” suggested for food allergy etc i cannot do because i would have nothing to eat. I cannot tokerate potato, rice, etc (long list)
So recapping on questions…hisramine vs tyramine determination, meaning of low blood histamine, and anything else tou have input on sorry for long message. Got carried away by the thoroughness of your post
Hi Sammi
Thank you for your post. Your symptoms and test results point to a compromised gut function, most likely gut wall damage, gut flora imbalances and potential intestinal parasites. That’s why you are reacting to so many random foods, therefore it’s unlikely that further food restrictions or analysing histamine/tyramine effects would help. I suggest you consider doing a comprehensive gut repair and healing treatment with an experienced practitioner as your food sensitivities go a long way back. GAPS nutritional protocol is very good under theses circumstances, it may take a few years of following it consistently to heal the gut and food intolerances, among others. See my post about it here: http://naturimedica.com/gaps-diet-what-is-it-and-when-to-apply-it-sydney-adelaide-australia/
Hello, I have a million questions! One is how can you tell if vitamins or medications have histamine in them? For example, looking at a box of disprin I can’t find it it does or doesn’t contain histamine. I’m also wondering about centrum multivitamins and neurofen tablets. Thanks!
Histamine is a natural substance produced by the body (it’s found in most body tissues) and is also present in many foods. There are foods that specifically increase release histamine release in the body as a response to an allergen such as inhalants (e.g. pollens, dust), medications (e.g. aspirin, penicillin) and stings (e.g. bee venom), among others. So drugs and supplements don’t contain histamine but the body may react to them by releasing histamine as a response to them which can cause itching, hives, rashes, congested sinuses, gut symptoms etc. Different people respond differently to foods and drugs so it’s usually trial and error method to identify the culprits specifically for you.
My 12 year old son have been suffering from birth with skin rash. About 3 years ago he started with a asmatic cough. Some seasons it is worse than others. He is constantly sniffing. He often complains that he is tired or that his head hurts. When he was 6 he was diagnosed with ADD. Could this all just be histamine intolerance? And if so, how can I treat it. The drs. always say it is either asma or alleries.
Have you done any food sensitivities/intolerances testing for your son? If not, I suggest you consider testing for these together with gut function testing (which is related to food sensitivities, ADD and asthma) plus vitamin D levels – also connected to food intolerances and the immune function in general. Constant sniffing may indicate dairy sensitivity, likely among others.
Hi Joanna thank you for your Web pages. Just a question regarding fresh food. Would you consider unused chopped fruit eaten hours or a day later as fresh or leftover? Same question for chopped or peeled vegetables? Thank you in advance. Claire.
Hi Claire
Thank you for your question. I’d consider these fruits and vegetables as leftovers with a diminished nutrition values. You can freeze any excess produce for future use.
Wow best article I have seen yet on histamines. There are many things that can cause mast cell activation syndrome. Untreated illnesses like Lyme or candida, GMOs destroy the gut and gut bacteria which can cause leaky gut which can cause it. Excitotoxin build up from vaccinations, food and our enviroment can build up and cause it.
Great article, thank you.
Thank you for taking the time to comment and for your feedback!
Hello Joanna,
I just got back from my first visit with an endocrinologist. I am male age 63. My main complaint is fatigue and insomnia. My Histamine Plasma level came back 137. I understand this may be high, please advise. The course I was told to follow is a low histamine diet along with B-12, omega 3 with Co Q10, digestive enzymes, probiotic (yeast) and DAO enzyme.
Also, Is there a correlation with adrenal exhaustion and or pancreatic cancer and high histamine levels?
Hello Mike
I’m afraid I’m not able to comment on the treatment/ supplements given to you by your endocrinologist. Adrenal glands are sensitive to toxins and gut bacteria imbalances so if you have histamine intolerance this means your gut bacteria is out of balance which would affect the adrenals. I’m not aware of any connections between adrenal fatigue, pancreatic cancer and high histamine.
Karen
Thank you for your email. From your short description of your son’s symptoms it may or may not be histamine intolerance in combination with some other factors. There are many possibilities that need to be checked and excluded. As you appreciate I can’t provide any specific advice without the full picture but have you looked at and/ or excluded the following:
– Mould exposure (past or present) – can manifest in hives
– Low grade viral infection
– Wearing clothes that have a lot of dye (such as cheaper black jeans) or washing powder/fabric softener, detergents
Treatment avenues:
– Homeopathy – a great option to consider, often works when nothing else seems to
– Focusing on improving the liver function for blood purification and toxins removal – this is a must in this case in my opinion
– Repairing, balancing and healing the gut – is the key to any improvements. Have your son done a tailored gut treatment?
There are histamine intolerance tests available, the NutriPath lab in Australia has a test and I’m sure there are labs in the US that do this s well. Functional medicine doctors/ practitioners may be better to talk to in such cases, you can find one in your area here: https://www.functionalmedicine.org/practitioner_search.aspx?id=117
Overall, keep going until you find a practitioner who can provide guidance in this complex case and will look into possible causes(s) to address this on a permanent basis.
All the best
Joanna
Sent: Wednesday, 10 August 2016 12:06 AM
To: joanna@naturimedica.com
Subject: Your article on over production of histamine
I tried to post this to the article but wasn’t successful. My 14 year old son has had chronic hives for five years and I have tried every possible natural solution such as the Elimination Diet, Acupuncture, seen a Naturopathic doctor, tumeric, pro biotics, vit. c, green juices, removed carpets , stuffed animals from house, hepa vacuum, use only natural shampoos, detergents, eat all organic, cook most from scratch for him. I have read book after book to help him to no avail. Regular allergists, doctors only want to give him a bandaid such as zyrtec or steroids (which we refuse). All of his many , many blood tests come back perfect. He cannot function if he doesn’t take one zyrtec a day as his body is covered head to toe in hives and his hands and feet often swell as well. Please tell me how I can get his doctor or how I can tell if he is deficient in the enzyme in your article DAO? Thank you! Please help if you can!
I have taken anti histamines for the last few years. Sinus problems, hayfever, prickly heat on hands, headaches, pins & needlesin fingers occasionally and now acid reflux in my throat. H Pylori was found in my gut too so I had antibiotics which I reacted to. Think i have high histamine levels. Not sure what I can eat as so much food is the problem but will take more supplements to hopefully correct imbalance and reduce need for antihistamines over the counter. Thank you for any response.
Denise
All symptoms you’ve described are connected to the gut health and function. Plus you had a course of antibiotics which also had a negative effect on the gut flora. Therefore I suggest you start from improving the integrity and function of your gut and digestion to commence the recovery process.
All the best
Joanna
Hi. I have dealt with skin itching while working out ever since I was a kid. It seems to run in my family. It does go away if you push through it and continue to exercise regularly. I started taking zyrtec and it fixed the problem. Needless to say once I go off of it I’m like a drug addict who’s trying to go clean. My skin starts itching without friction. Is there a special Doctor that would be able to assist me in starting the regimen? Also my skin is overly sensitive to products and insect bites. Thank you
Hi Jan
I suggest you embark on a gut and digestion balancing program with a naturopath or a functional medicine practitioner who can conduct a few test (which ones will depend on your specific symptoms) to pinpoint the imbalances.
Hi Joanna,
I have a histamine intolerance since I can remember, I limit my diet and don’t eat foods that I know set me off, anything with Yeast, sugar, citrus, chocolate, tomatoes, I limit alcohol to preservative free red wine, now I am early stages of pregnancy I am wondering if the daily prescribed antihistamine I have taken for years is doing my gut flora real harm and I will then pass on my intolerances to my child. Do you have any further advice on the direction I should travel with this? or can you recommend a naturopath in Perth WA that I can contact? Thank you
Hi Danielle
Needless to say Iit’s best to do any gut repair and gut flora balancing well before the pregnancy because not many supplements/ medications can be used whilst you are pregnant. You can only pass to your child the gut flora you currently have or will have at birth. I agree it’s best to talk to a local natural medicine practitioner about what can be done now and in the future. Unfortunately I don’t know of any practitioners in Perth to suggest. Looks to me like you’ll need to embark on a comprehensive gut cleanse and repair program in the future (after pregnancy and lactation period is over) to deal with the histamine intolerance you’re experiencing.
Joanna,
Your article has truly been eye opening. For the last several years I have been experiencing what can only be described as a food allergy, causing symptoms ranging from bloating, gas, heartburn, you name it. I’ve tried eliminating certain foods to see what helps and what doesn’t, but have not been able to locate any common link. Something I can eat once, the next time makes me sick. As you can imagine, this makes it very difficult to know what to eat.
Further complicating things is that anytime I bring any of this up to doctors, especially in that it seems to cause anxiety, ongoing sinus type issues, acne, etc, I am constantly brushed off, and assured that it must all be in my head. Thus I continue feeling bad, with brief moments of feeling good.
My question for you would be what type of specific Doctor do I need to see if I suspect a histamine intolerance might be the root of my issues? My pcp seems convinced I have Gerd and just prescribes medication that I’m not willing to take, as my symptoms don’t meet fully a Gerd diagnosis. I’ve been to a gastroenterologist who tested my gallbladder, and there was no issue there. My endocrinologist monitors my thyroid and blood sugars, all of which are within range, though cholesterol is always on the higher end. Who can I see to help determine if this is an issue for me, and what tests should I request? Thank you for any guidance you may have.
Brandon
Thank you for your post. From your short description I’d say you need to embark on the gut healing program backed by tests, including complete digestive stool analysis, SIBO and organic acids, to pinpoint what imbalances are present. Histamine intolerance tests are also available but it’s a relatively new field. In Australia lab called Nutripath does it. I find that a comprehensive gut repair and healing treatment combined with nutrition often addresses histamine issues as well.
I suggest you look for a functional doctor in your area who understands digestive complaints and can refer for and interpret the tests. Just Google ‘functional medicine practitioner” plus your location.
All the best
Joanna
Hi Joanna
I’ve had a Comprehensive Parasitology Test carried out and have been advised to take a course of Biocare BioAcidophilus Forte Plus and Higher Nature Oregano Oil. I have histamine intolerance and was wondering if you could tell me whether these items would be suitable to take?
Thanks Joanna.
Regards,
Hilary.
Hi Hilary
Did your test included testing for histamine intolerance? It’s not common for even comprehensive parasitology tests to test for it and separate histamine intolerance test is required from my experience practising in Australia, although UK may be different. It’s hard for me to comment on these particular supplements prescribed/suggested by your practitioner not knowing the full picture.
I do have a comment that should be useful for you: oregano oil is a strong antimicrobial and is usually taken for a few weeks and then break is needed (depending on the dose, of course). It kills both good and problematic bacteria therefore I usually prescribe it on its own or together with other antimicrobials, and then follow up with probiotics. If oregano oil and probiotics are taken together, which is also a viable strategy depending on the case, you need to take them well apart e.g. oregano oil in the morning and/or lunch and probiotics at dinner or before bed. However, it’s best to discuss the options with you practitioner for the most effective treatment.
Hope this helps
Joanna
Hi Joanna
wow this is a very interesting,I have change me diet over the last 12 months eating healthy,after having half of my thyroid removed last year,to a multinodular goitre.
more eggs more yogurt and alot more foods that are on your list,and now i’m getting tested as my ACTH level are high,most of the systems i have are on your list,could having histamine intolerance be my issue and be giving me a high ACTH reading??
kind regards Tracey
Hi Tracey
If your ACTH levels are high you need to do further testing to help determine the cause. Your gut/ histamine intolerance symptoms may or may not be related.
All the best
Joanna
Hi, my family has started on the GAPS program. 2 weeks in and everyone is enjoying the food :) I have found your article while I was researching about my husband’s hives. This condition is not new since starting the diet. He can have it for months and then it goes away for a few years and then overnight its back with a vengeance. This current episode has been going since Feb/March this year. Our doctor treated it with anti-histamine tablets and phenergyn (both of which he was taking multiple times a day for a few weeks – not good I know). He would be covered from head to toe and these tablets could take 2 hours to reduce his skin swellings and itchiness. We haven’t been able to find food triggers to it but he is a shiftworker so loses a lot of sleep and is morbidly obese in weight (we have previously found he drops weight quickly when we remove grains and starches from his diet – don’t know if that is a clue but GAPS is doing wonders. He says he’s feeling great on it). It has been suggested that he take a probiotic of Lactobacillus rhamnosus GG to help his gut flora in breaking down the histamines. Would this be a short term or long term treatment? Would this strain be enough on its own? Would a CSDA be necessary? Would appreciate your thoughts before we go spending hard earned money.
Hi there
I would include more probiotic strains that are indicated for histamine intolerance in addition to LGG such as Bifidobacterium infantis, Lactobacillus Plantarum, ideally in one supplement.
Depending on the test type, CDSA will not cover histamine intolerance (there are specific tests for this) but will show the balance and levels of good and problematic bacteria, parasites and any digestive issues with protein, carbs and fat.
GAPS diet will help with histamine intolerance, and if followed consistently and long enough, should resolve the issue in time.
I’m looking for a brand of probiotic for treatment of histamine intolerance and or amine intolerance.
Catherine
I mentioned a few specific probiotics in my article here:
“Histamine-degrading bacteria (probuiotics) include bifidobacteria species, but particularly Bifidobacterium infantis, Lactobacillus Plantarum, Lactobacillus rhamnosus, salivarius, and Lactobacillus gasseri (1)”
All the best
Hi Joanna,
I think I might have a histamine problem. I have seen my GP and a skin specialist who said that I have Chronic Urticaria but I dont get any rashes. I have a problem with itchy skin starting on my head and over about half a day it moves down to my shoulders and to my arms. It feels like my skin is burning and it becomes red. The specialist told me that my body produces too much histamine and it comes out through the pores in my skin making me itchy. He also told me that there is no cure and that hopefully one day it will just go away. I take an anti-histamine tablet every day and have been doing this for about 6 years. This is the only relief I get from it. As long as i take the tablet daily I am ok. For the past 2 years I have been able to go 2 days without the tablet but I am worried that the tablet is doing me damage. I dont know what to do about it or who to see.
I also get chronic headaches occasionally which cause me to vomit. I dont know if this is related. I have suspected a caffeine addiction.
Who or what can I do to find out if I have a gut problem causing a histamine intolerance. I am suspecting either coffee or dairy products. Last year I was sick for about 2 weeks and didnt eat or drink either. I didnt need to take a tablet for about 3 weeks.
From the web site address I presume your not in Australia so I cant make an appointment to see you.
Could you please offer me some advise on what I can do or who I can see.
Thank you for the article and any help you can offer.
Hi Jon
I’m based in Australia (Sydney at present). I’ll send you an email to your private address to discuss this further.
All the best
Joanna
Thank you for the article which is useful in confirming I have an underlying symptom of histamine intolerance (I have/had 7 of the symptoms). Unfortunately the problem makes me vulnerable to allergic reaction anaphylaxis (wasp-sting). I have had 4 events, the 3rd fixed in hospital, the 4th with an epi-pen. Now I noticed after applying the epi-pen the recovery was immediate and complete, suggesting a shortage of adrenaline. It seems the body tries to normalise the histamine level with body made adrenaline, so when an allergic challenge occurs there is no reserve available to handle it. In STOP AMERICAS #1 KILLER, there is a chapter on Histamine and VitaminC deficiency, which says “histamine levels in blood are inversely related to blood levels of vitamin C”. So I started taking 1.5mg of Ester-C daily, and since then have had 3 confirmed sting events without anaphylaxis. In the last event bp rose from about 110 to 174, pulse from 50 to 74.
Now the question is should I do anything more than the vitamin C. I do get bp about 90 occasionally and pulse 45 – I am 76. I should add that neither the hospital or my GP ever mentioned histamine intolerance and seemed to think I was stuck with the epi-pen!
George
Thank you for taking the time to comment. Vitamin C increases histamine degradation and removal in the gut thus lowering histamine levels. You may want to experiment with higher vitamin C doses and see if increased daily dose works even better for you. You may also consider adding vitamin E (full spectrum one containing both tocopherols and tocotrienols) which stabilises mast cells (they secrete histamine), vitamin E and vitamin C work together potentiating their effects on histamine and as antioxidants protecting against free radical damage; and specific probiotics such as Bifidobacterium infantis, Lactobacillus plantarum or soil-based probiotics to further support the gut and the immune system.
All the best
Joanna
to GEORGE ATKINSON Have just read your Vitamin C suppliment and also .. did you learn any more about the Adrenalin theory. ? I am a fellow sufferer Many thanks..Ross
Hi there, I am on a gut healing plan. I just started taking probiota bifido but the next day my histamine reactions are horribly. Do you think it could be die off? Thank you,
Hi Kailyn
In histamine intolerance there are significant imbalances of the gut flora (dysbiosis) potentially leading to SIBO (small intestine bacterial overgrowth). Often there is overgrowth of both ‘good’ and ‘bad’ bacteria including bifido bacteria. So if you have bifido overgrowth and supplement with it, this will further imbalance the gut and symptoms will intensify. The best way to be sure which types of gut flora are out of balance is to do the stool test such as CDSA (Complete Digestive Stool Analysis) and then supplement with the right probiotic and diet to balance the gut flora.
Hope this helps.
All the best
Joanna
Hiya i thinm i have a histamine intollerance because i have a yeast problem. Is this possible?
Yes, it’s possible as having yeast overgrowth causes imbalance of bacteria in the gut that may cause overgrowth of the histamine producing bacteria causing intolerance symptoms. As you gut health improve, histamine intolerance should lessen or disappear.
All the best
Joanna
Will the treatment with a rife machine bring the ant-histamine ude down
Hi there
I’m aware of various rife machines but not really familiar how they work. Having said this, I have one patient with complex gut issues, including histamine intolerance, who is using her rife machine to deal with gut pain. She says it really helps her. So perhaps it’s worth trying to see if it works for you in addition to a gut healing program.
All the best
Joanna
I have just read your posting, very interesting indeed. I have always suffered from severe excema – the itching and beyond dry skin is worsening all the time, but in the last year my face is becoming more and more affected by becoming very red and stinging. It is so embarrassing and extremely painful and making my life very depressing as impossible to mask with makeup.
I seem to have the intolerance to histamine from research. I have tried gluten free but on looking at what you can and cannot eat it appears nothing – o dear. I do eat healthily, well I thought I did but would love your advice. I am 63 and very conscious of grooming and looks and this is ,like I said become intolerable. Many many thanks – cheers Louise
Hello Louise
Thank you for reading and taking the time to comment. I’m glad my post helped you to look at other possible cause(s) of your symptoms. Please let me know how you go implementing the above.
All the best
Joanna